Knee Replacement Surgery: Modern Techniques and What Patients Should Know
Explore the latest advances in knee replacement surgery, from robotic-assisted procedures to rapid recovery protocols. Learn what modern techniques mean for your surgery and recovery.
Introduction
Knee replacement surgery has evolved dramatically over the past decade, with new techniques offering patients better outcomes, shorter recovery times, and improved long-term function. Whether you're dealing with severe arthritis, injury, or degenerative joint disease, understanding modern knee replacement options can help you make informed decisions about your care.
This comprehensive guide explores the latest surgical techniques, what to expect, and how these advances benefit Medicare patients seeking knee replacement surgery.
The Journey to Your New Knee: Understanding Your Options
When knee pain begins controlling your life rather than the other way around, the conversation about knee replacement surgery inevitably begins. But here's something that might surprise you: not all knee replacements are created equal, and the choice between different approaches can dramatically impact everything from your recovery timeline to how your new knee feels years down the road.
The decision between total and partial knee replacement isn't just a medical one—it's deeply personal, affecting how quickly you'll return to the activities you love and how natural your knee will feel as you navigate daily life. Let's explore what each option really means for you.
When Your Entire Knee Needs a Fresh Start
Total knee replacement represents the complete transformation of your knee joint. Think of it as renovating your entire kitchen rather than just replacing a broken appliance. When arthritis has damaged multiple areas of your knee, or when years of conservative treatments have simply stopped working, total replacement offers a comprehensive solution.
This approach involves replacing all the major surfaces of your knee joint with carefully engineered artificial components made from advanced materials like titanium and medical-grade plastics. The result is a knee that moves smoothly without the bone-on-bone grinding that causes so much pain in severe arthritis.
The Minimalist Approach: Partial Knee Replacement
But what if only one area of your knee is causing problems? This is where partial knee replacement shines. Imagine if you could fix just the damaged part of your knee while leaving everything else untouched—that's exactly what partial replacement offers.
This targeted approach preserves your healthy bone, cartilage, and ligaments, working with your body's existing structures rather than replacing them. The benefits extend far beyond the operating room. Your incision will be smaller—typically 3-4 inches compared to the 6-8 inches needed for total replacement. Your recovery moves faster because your surgeon isn't disrupting as much tissue. Most importantly, many patients report that their partial replacement feels more natural, almost like their original knee before arthritis took hold.
The preserved ligaments continue doing their job of providing natural feedback and stability, which often translates to better range of motion and a more intuitive feeling when you walk, climb stairs, or return to recreational activities.
What This Means for Your Medicare Coverage
The good news for Medicare beneficiaries is that both approaches receive the same level of coverage when medically necessary. Your out-of-pocket costs typically range from $1,500 to $4,000, depending on your specific Medicare plan and any supplemental coverage you may have. The decision between total and partial replacement should be based entirely on what's best for your knee, not financial considerations.
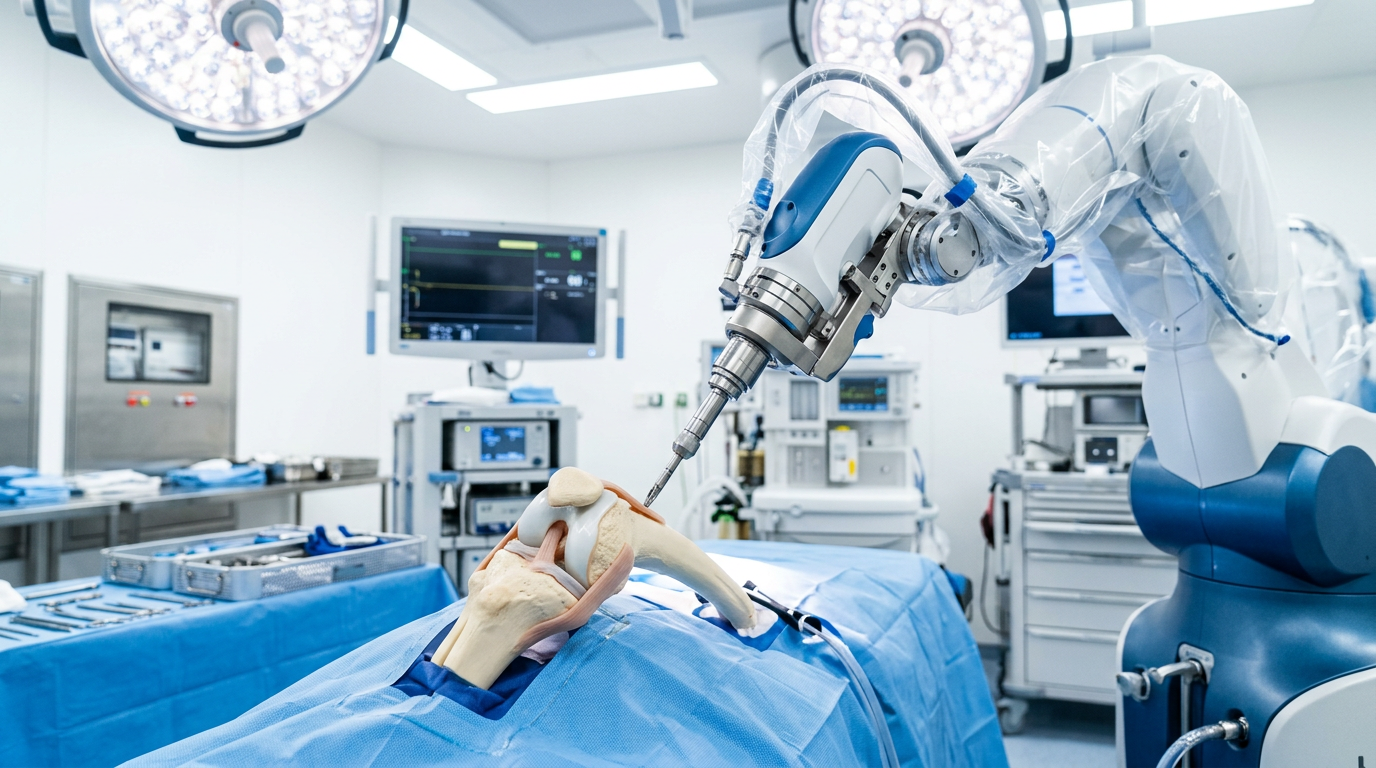
The Robot in the Operating Room: How Technology is Revolutionizing Knee Surgery
If someone had told you a decade ago that a robot would help perform your knee replacement surgery, you might have imagined something from a science fiction movie. Today, robotic-assisted surgery has become one of the most exciting developments in orthopedic care—and it's changing the game for patients who want the most precise, personalized treatment possible.
But here's what might surprise you: the robot isn't actually performing your surgery. Instead, it's working as your surgeon's most sophisticated assistant, providing unprecedented precision and planning that simply wasn't possible with traditional techniques.
Planning Your Surgery Before You Even Arrive at the Hospital
The robotic revolution begins weeks before your surgery, in the quiet hum of an advanced imaging suite. Using detailed 3D CT scans, systems like the MAKO and ROSA platforms create a digital twin of your knee—a virtual model so precise that your surgeon can examine every bone surface, measure every angle, and plan every cut before making the first incision.
This isn't just impressive technology for technology's sake. This digital planning phase allows your surgeon to select the perfect implant size, determine the optimal positioning, and map out the surgery in a way that's uniquely tailored to your anatomy. Think of it as having a detailed blueprint before building your dream home, except this blueprint is designed specifically for your knee.
Millimeter-Perfect Precision Where It Matters Most
During the actual surgery, this is where the magic happens. The robotic arm doesn't work independently—it's more like a highly sophisticated guidance system that helps your surgeon achieve millimeter-level accuracy that human hands simply can't match consistently.
As your surgeon works, the robotic system continuously monitors the procedure, ensuring that every bone cut and every implant placement matches the pre-planned specifications exactly. If your surgeon's hand moves even slightly outside the planned parameters, the system provides gentle resistance—like bumpers on a bowling lane, keeping everything perfectly on track.
This precision translates into real benefits you'll feel long after you've recovered. Better implant positioning means improved joint mechanics, which often leads to a more natural feeling knee and potentially longer implant life. The system also helps preserve more of your healthy bone and tissue, which can contribute to faster healing and better long-term outcomes.
The Best News: Medicare Has Your Back
Here's something that often surprises patients: Medicare covers robotic-assisted knee replacement at the same level as traditional surgery. When performed at Medicare-approved facilities, you won't pay extra for choosing this advanced technology. The procedure uses the same billing code (27447) as conventional knee replacement, meaning your out-of-pocket costs remain the same whether you choose robotic assistance or not.
When Full Robotics Isn't Available: Computer Navigation Steps In
Not every hospital has a full robotic system, but that doesn't mean you have to settle for outdated techniques. Computer navigation systems offer many of the same precision benefits, providing real-time guidance that helps surgeons achieve better implant alignment and improved outcomes.
These systems work like a GPS for your surgery, continuously tracking the position of surgical instruments and providing instant feedback to ensure optimal implant placement. While not as comprehensive as full robotic assistance, computer navigation still represents a significant advancement over traditional freehand techniques, offering improved accuracy and better long-term results.
Your Surgery Day and Beyond: How Modern Approaches Are Changing Recovery
The days of lengthy hospital stays and months of painful recovery are becoming a thing of the past. Today's knee replacement surgery looks dramatically different from what your friends or family members might have experienced even five years ago, with innovations that can get you back on your feet faster than you might imagine.
The Evolution from Marathon to Sprint
Traditional knee replacement surgery used to feel like running a marathon—a long, challenging journey that required significant endurance. The surgery itself typically took 60-90 minutes, followed by 2-3 days in the hospital as you slowly worked through the initial recovery phases. Most patients needed 6-12 weeks before feeling comfortable returning to their normal activities, with physical therapy beginning the day after surgery.
While this approach still works well for many patients, it's no longer the only option available.
The Minimally Invasive Revolution
Minimally invasive techniques have transformed knee replacement from a marathon into more of a sprint. These approaches reduce surgery time to 45-75 minutes and can slash hospital stays to just 1-2 days. Some procedures are now even performed on an outpatient basis, allowing you to recover in the comfort of your own home rather than a hospital room.
The benefits extend far beyond shorter hospital stays. Because minimally invasive techniques involve smaller incisions and less disruption to surrounding muscles and tissues, your body can focus more energy on healing rather than dealing with unnecessary surgical trauma. This often translates to a recovery timeline of 4-8 weeks instead of the traditional 6-12 weeks, and physical therapy can often begin the same day as your surgery.
The Game-Changer: Enhanced Recovery Protocols
Perhaps the most exciting development in knee replacement isn't a surgical technique at all—it's a complete reimagining of the entire treatment process. Enhanced Recovery After Surgery (ERAS) protocols represent a comprehensive approach that optimizes every aspect of your experience, from the moment you decide to have surgery through your complete recovery.
These protocols begin with pre-operative conditioning and education that prepares your body and mind for surgery. Instead of simply showing up on surgery day, you become an active participant in your recovery from the very beginning. Multimodal pain management strategies use multiple approaches to control discomfort, often reducing reliance on opioid medications while providing better pain control.
Early mobilization techniques get you moving safely within hours of surgery, helping prevent complications and accelerate recovery. Perhaps most importantly, coordinated discharge planning ensures that your transition from hospital to home is seamless, with all the support and resources you need already in place.
The results speak for themselves: ERAS protocols can reduce hospital stays by 1-2 days and speed overall recovery by 2-4 weeks compared to traditional approaches. More importantly, patients often report feeling more confident and prepared throughout the entire process, knowing exactly what to expect at each stage of their journey.
What Success Really Looks Like: Real Expectations for Your New Knee
Let's talk honestly about what you can expect after knee replacement surgery, because managing expectations is just as important as managing your recovery. The good news is overwhelmingly positive, but understanding the realistic timeline and outcomes will help you approach your surgery with confidence and patience.
The Numbers Tell an Encouraging Story
Modern knee implants have a track record that would make any manufacturer proud. Ninety-five percent of implants are still functioning well at the 10-year mark, and an impressive 85-90% continue performing effectively even at 20 years. These aren't just statistical victories—they represent decades of pain-free mobility for the vast majority of patients.
But perhaps more meaningful than implant longevity is patient satisfaction. Consistently, 85-90% of knee replacement patients report being satisfied or very satisfied with their decision to have surgery. This high satisfaction rate reflects something profound: the substantial improvement in quality of life that most patients experience after their recovery is complete.
Getting Back to the Life You Love
One of the most common questions patients ask is, "What will I be able to do with my new knee?" The answer is more encouraging than many people expect. Most patients find they can return to a full range of low-impact activities that bring joy and fulfillment to their lives.
Walking becomes a pleasure again rather than a painful necessity. Swimming offers excellent exercise without stressing your new joint. Cycling—whether on the road, trail, or stationary bike—provides great cardiovascular benefits and is typically very well tolerated. Golf enthusiasts are usually delighted to find they can return to the course, often with less pain than they've experienced in years.
Daily activities that may have become challenging—like confidently navigating stairs, spending time in the garden, or enjoying light hiking—typically become manageable again within a few months of recovery. Most patients find they can return to work within 6-12 weeks, depending on the physical demands of their job.
The Activities That Require a Different Approach
While your new knee will likely exceed your expectations in many ways, it's important to understand that some activities require careful consideration or modification. High-impact sports like running and basketball can place excessive stress on your implant, potentially shortening its lifespan. This doesn't mean you have to become sedentary—it means choosing activities that love your knees back.
Activities with increased fall risk may require extra caution or modification as you adapt to your new joint. Regular heavy lifting over 50 pounds isn't necessarily prohibited, but it should be approached thoughtfully and discussed with your surgeon based on your specific situation and needs.
When Surgery Might Be Recommended
Conservative Treatment Options to Try First
Before considering surgery, most doctors recommend a comprehensive conservative treatment approach including physical therapy and exercise, weight management, anti-inflammatory medications, corticosteroid injections, hyaluronic acid injections, and activity modification.
Clear Indicators for Surgery
Surgery may be appropriate when pain significantly limits daily activities, conservative treatments have failed after 3-6 months, X-rays show significant joint damage, sleep is regularly disrupted by knee pain, or quality of life is substantially impacted.
Life After Knee Replacement
Immediate Recovery (0-6 weeks)
The initial recovery phase focuses on reducing swelling and regaining basic mobility through physical therapy 2-3 times per week. Patients typically return to driving after 2-4 weeks and may use assistive devices as needed during this period.
Medium-term Recovery (6 weeks - 6 months)
This phase emphasizes continued strength building and range of motion work as patients return to work and most daily activities. Low-impact recreational activities can begin during this time, while ongoing monitoring for complications remains important.
Long-term Success (6+ months)
Long-term success involves full return to approved activities, annual follow-ups with your orthopedic surgeon, ongoing exercise to maintain joint health, and weight management to ensure implant longevity.
Making the Right Decision
Questions to Ask Your Surgeon
- What type of implant do you recommend and why?
- Are you experienced with robotic-assisted surgery?
- What is your infection rate and revision rate?
- What does your rapid recovery protocol include?
- How many knee replacements do you perform annually?
Medicare Coverage Considerations
- Medicare covers both traditional and robotic-assisted knee replacement at the same rate
- Typical out-of-pocket costs: $1,500-$4,000 depending on your plan
- Ensure your surgeon accepts Medicare assignment
- Verify the facility is Medicare-approved
- Physical therapy and home health services are typically covered when medically necessary
Finding Your Surgical Champion: How to Choose the Right Knee Replacement Surgeon
Choosing your knee replacement surgeon is one of the most important decisions you'll make in this journey, and it deserves more thought than picking a restaurant for dinner. The right surgeon doesn't just perform excellent surgery—they become your partner in achieving the best possible outcome for your unique situation.
The Questions That Really Matter
When interviewing potential surgeons, go beyond asking about their credentials (though those matter too). Ask about their experience with your specific type of procedure. A surgeon who performs 200 knee replacements annually will have refined skills and troubleshooting abilities that can make a real difference in your outcome.
Don't be shy about asking for their personal statistics. What's their infection rate? How often do they need to perform revision surgeries? These numbers should be readily available and significantly better than national averages. A surgeon who's reluctant to share their outcomes data may not be the right choice for your care.
Perhaps most importantly, ask about their approach to recovery and pain management. Do they use enhanced recovery protocols? Are they experienced with robotic or computer-assisted techniques? How do they handle complications when they arise? The answers will give you insight into whether their philosophy aligns with your expectations and goals.
The Medicare Advantage
As a Medicare beneficiary, you have some unique considerations when choosing your surgeon. Verify that your surgeon accepts Medicare assignment and that the surgical facility is Medicare-approved. Understanding your out-of-pocket costs upfront prevents surprises later and helps you budget appropriately for your care.
Ask specifically about coverage for physical therapy and home health services, as these can be crucial components of your recovery. Some surgeons work closely with rehabilitation providers who specialize in Medicare patients, which can streamline your care coordination.
Your Path Forward
Modern knee replacement surgery offers excellent outcomes with 85-90% patient satisfaction rates. The key to success is choosing an experienced surgeon, understanding your options, and having realistic expectations about your recovery timeline.
Taking the Next Step
If conservative treatments haven't provided adequate relief and knee pain is limiting your quality of life, start by:
- Consulting with an orthopedic surgeon who specializes in knee replacement
- Asking about modern techniques like robotic assistance or minimally invasive approaches
- Understanding your recovery timeline based on the specific procedure type
- Verifying Medicare coverage and out-of-pocket costs upfront
- Getting a second opinion if you're unsure about recommendations
Don't let fear or misconceptions prevent you from exploring your options. With today's advanced techniques and enhanced recovery protocols, most patients find the anticipation is worse than the reality.
This article is for informational purposes only and should not be considered medical advice. Always consult with qualified healthcare professionals for medical decisions.
References
[1] Centers for Medicare & Medicaid Services. (2025). CY 2025 Medicare Hospital Outpatient Prospective Payment System. Retrieved from https://www.cms.gov/medicare/medicare-fee-for-service-payment/hospitaloutpatientpps
[2] Medicare Payment Advisory Commission. (2025). Report to the Congress: Medicare Payment Policy. Retrieved from https://www.medpac.gov/document/report-to-the-congress-medicare-payment-policy-march-2025/
[3] American Academy of Orthopaedic Surgeons. (2025). Total Knee Replacement Guidelines and Best Practices. Retrieved from https://www.aaos.org/quality/quality-programs/joint-replacement/
[4] Centers for Medicare & Medicaid Services. (2025). Medicare Coverage Database: Knee Replacement Procedures. Retrieved from https://www.cms.gov/medicare-coverage-database/
[5] Journal of the American Medical Association. (2024). Outcomes in Modern Knee Replacement Surgery. Retrieved from https://jamanetwork.com/journals/jama/
[6] New England Journal of Medicine. (2024). Robotic-Assisted Joint Replacement: Clinical Outcomes and Patient Satisfaction. Retrieved from https://www.nejm.org/